When a person loses a limb, their world changes overnight. Every movement, every habit, even their sense of balance must be rebuilt from the ground up. For doctors, that moment marks not the end of surgery but the beginning of something just as critical—the journey toward mobility.
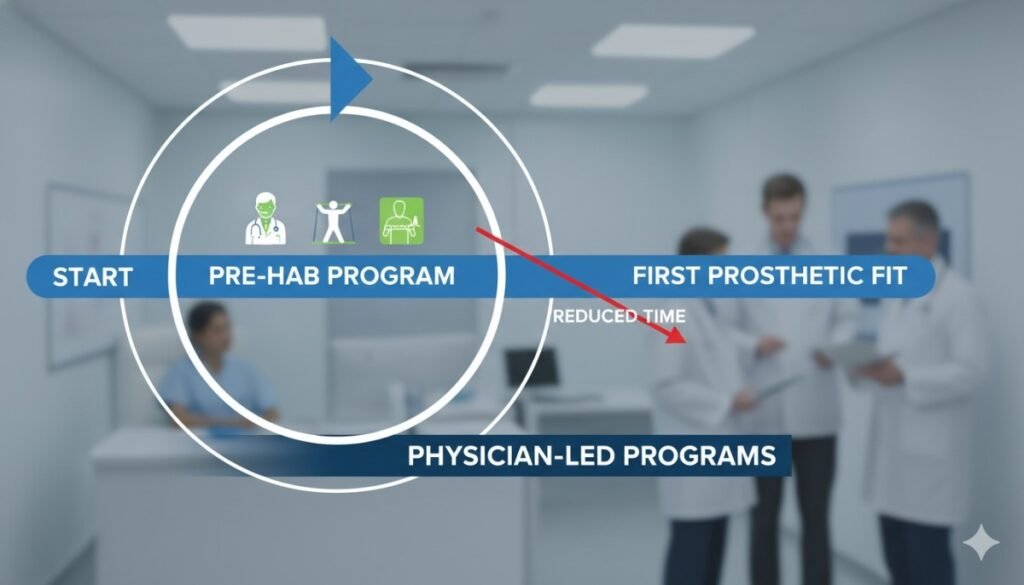
Traditionally, most of the focus in prosthetic care begins after surgery. But what if the real secret to faster recovery actually starts before the first fit?
That’s where pre-habilitation—or “pre-hab”—comes in. Pre-hab is a structured, physician-led program designed to prepare the body and mind for prosthetic success even before the device is fitted. It focuses on strengthening muscles, improving flexibility, maintaining range of motion, and building confidence early.
For patients, this means shorter recovery times, fewer complications, and smoother transitions to walking or grasping again. For doctors, it means predictable outcomes, better socket fit, and stronger long-term satisfaction.
In this article, we’ll explore how pre-hab transforms recovery, what physician-led programs look like in action, and why India’s medical community is beginning to see it as an essential part of modern prosthetic care.
Because when preparation meets technology, the first step comes much sooner.
Understanding Pre-Habilitation in Prosthetic Care
What Is Pre-Hab?
Pre-habilitation, often shortened to pre-hab, is a proactive medical program that prepares patients for prosthetic rehabilitation before they ever receive their first device.
It focuses on physical conditioning, mental readiness, and lifestyle adaptation during the recovery phase after amputation but before prosthetic fitting.
Instead of waiting for healing to complete and then starting therapy, doctors use this time to build the foundation for success—keeping muscles strong, joints flexible, and the mind motivated.
The Goal of Pre-Hab
The main goal is simple: to shorten the time between amputation and prosthetic use.
By starting early, patients avoid the decline in strength, balance, and endurance that often occurs during inactivity. When the time comes for fitting, their body is already prepared, reducing complications and speeding up adjustment to the new limb.
In short, pre-hab bridges the gap between surgery and mobility.
Why It Matters So Much
Without pre-hab, many patients lose muscle tone and range of motion, making their first prosthetic experience painful and slow.
Their bodies are unprepared to bear weight or coordinate movement. The result is frustration, prolonged therapy, and sometimes even rejection of the prosthesis.
Pre-hab flips this narrative by keeping the body active and ready for progress. It turns waiting into training.
The Role of Physicians
Doctors play the most crucial role in pre-habilitation. They guide the process, monitor recovery milestones, and customize exercises based on each patient’s condition.
Physicians also coordinate with physiotherapists, prosthetists, and psychologists to ensure every aspect of recovery—physical, emotional, and functional—is aligned.
In physician-led pre-hab programs, every activity is goal-oriented and clinically justified, ensuring safe but progressive preparation.
How Pre-Hab Works
The Early Start
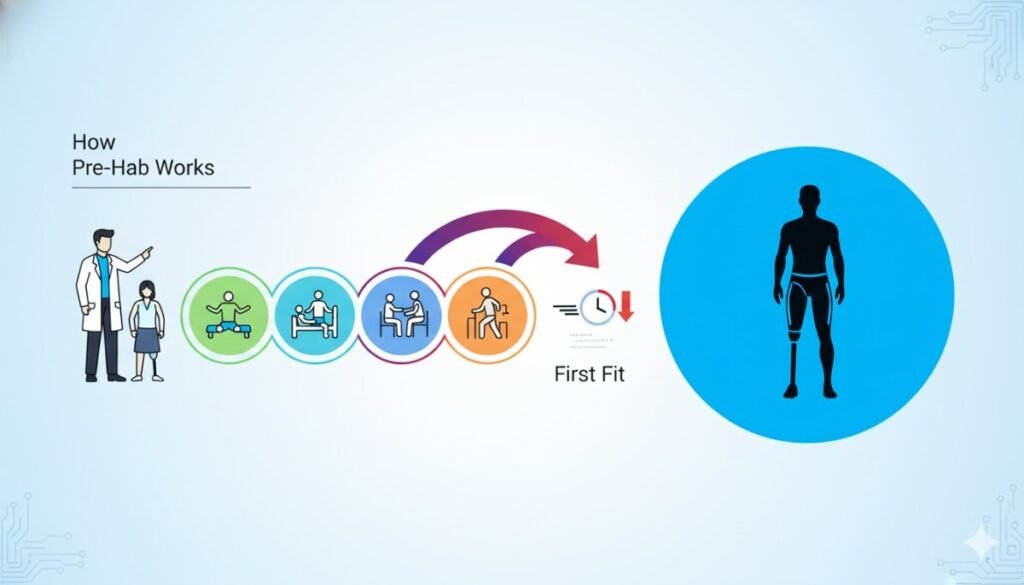
Pre-hab usually begins soon after surgery, once the wound is stable and cleared for light activity.
Doctors often begin with gentle movements or isometric contractions—simple exercises that keep blood flowing and prevent stiffness.
Even small, controlled movements at this stage have powerful effects. They preserve joint mobility, prevent muscle shortening, and signal the brain that movement is still possible.
Restoring Circulation and Healing
Physical activity during pre-hab improves blood flow, which supports tissue healing and prevents complications like edema and infection.
Physicians carefully balance activity with rest, ensuring that exercises never compromise wound closure or skin integrity.
In fact, patients who begin light pre-hab early often report fewer post-surgical complications and smoother socket fitting later.
Reconnecting the Brain and Body
After amputation, the brain must learn to understand the body’s new structure. Pre-hab exercises stimulate this neuroplasticity—the brain’s ability to adapt and reorganize.
Through guided movement and mirror therapy, patients start to rebuild body awareness, preparing for the coordination that prosthetic control will soon require.
This mental preparation makes prosthetic training faster and more intuitive.
Preventing Muscle Atrophy
In the weeks after surgery, unused muscles weaken quickly. Pre-hab combats this decline through targeted activation.
Simple exercises like limb lifts, core strengthening, and resistance band training help maintain the muscle groups that will support prosthetic use later.
For lower-limb amputees, this means strengthening hip extensors, glutes, and the sound leg. For upper-limb amputees, shoulder and trunk control become key.
Improving Balance and Stability
Amputation shifts a person’s center of gravity. The body must relearn balance—especially for those with lower-limb loss.
Pre-hab includes exercises that retrain posture, stability, and weight distribution using simple tools like therapy balls, standing supports, or balance boards.
By the time the prosthesis is fitted, patients already have a sense of control and coordination, reducing the fear of falling.
The Science Behind Early Preparation
The Principle of Neural Plasticity
The human brain constantly rewires itself in response to new challenges. After amputation, it begins to reorganize motor and sensory pathways.
Pre-hab takes advantage of this critical window. When movement is encouraged early—through exercise, visualization, or EMG (electromyography) training—the brain forms new neural connections faster.
This mental conditioning allows patients to adapt more smoothly when controlling their prosthetic later, especially for myoelectric systems that rely on muscle signals.
Muscle Memory and Coordination
Muscle memory doesn’t vanish after amputation—it just needs retraining.
During pre-hab, patients relearn how to move intentionally and consistently. These repetitions create stored movement patterns in the nervous system, which make prosthetic control feel more natural later.
Early repetition builds confidence. Patients stop fearing movement and start trusting their body again.
Psychological Readiness
Amputation doesn’t just affect the body—it challenges identity, confidence, and self-worth.
Pre-hab provides emotional structure during a vulnerable time. Doctors use this phase to offer counseling, introduce support groups, and set realistic recovery expectations.
By keeping patients engaged and goal-oriented, physicians prevent emotional withdrawal—a common barrier to successful rehabilitation.
The Role of Hormones and Circulation
Physical activity during pre-hab stimulates the release of endorphins and growth hormones. These chemicals not only lift mood but also accelerate tissue repair and muscle regeneration.
Regular movement keeps joints lubricated, reduces swelling, and helps maintain metabolic health—all of which are vital before fitting a prosthesis.
The Energy Efficiency Factor
Patients who go through pre-hab generally use less energy once they begin walking with a prosthetic.
Their strengthened core and balanced posture reduce fatigue, making prosthetic use more sustainable. This efficiency translates into better endurance and overall quality of life.
Physician-Led Pre-Hab Protocols
Phase One: Immediate Post-Operative Care
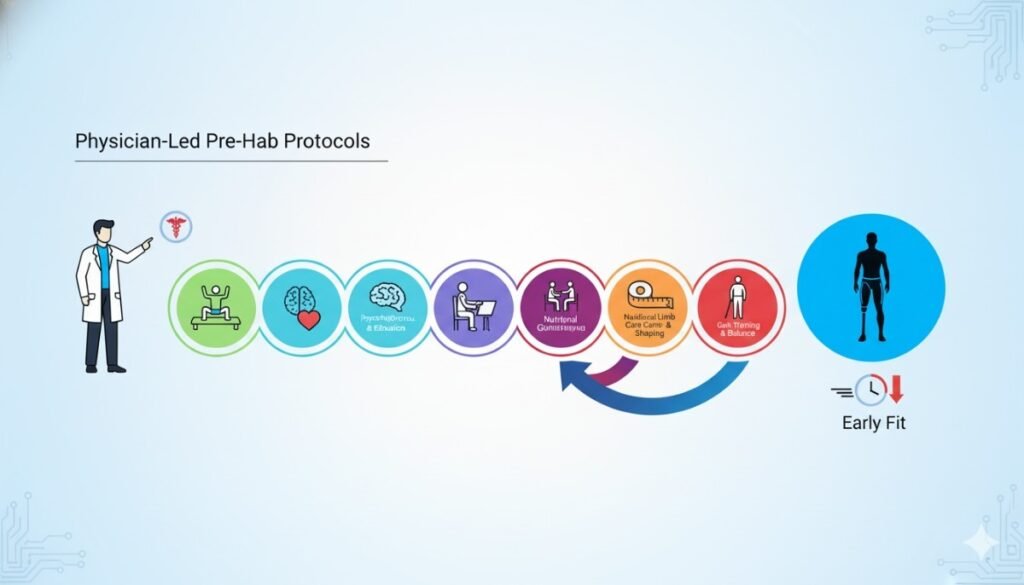
Right after amputation, the goal is to protect the wound while keeping nearby joints and muscles active.
Physicians prescribe gentle movements like ankle pumps, quad sets, or arm raises, depending on the limb affected.
They also ensure proper stump positioning to prevent contractures—permanent shortening of muscles that can complicate prosthetic fitting later.
During this phase, emotional reassurance is key. Patients are introduced to the concept of pre-hab and made to understand that early motion is safe and beneficial.
Phase Two: Controlled Mobilization
As healing progresses, doctors gradually increase exercise intensity.
They introduce light resistance, core strengthening, and partial weight-bearing activities under supervision.
This phase also includes early balance training, posture correction, and breathing exercises to improve endurance.
For upper-limb amputees, this stage focuses on shoulder mobility and bilateral coordination. For lower-limb cases, emphasis shifts toward standing tolerance and gait readiness.
Phase Three: Pre-Prosthetic Preparation
Once the wound is fully healed, physicians coordinate with prosthetists to begin stump conditioning and desensitization.
This involves gentle massage, compression wrapping, and skin care routines to prepare the residual limb for socket pressure.
Strength training becomes more dynamic, focusing on the specific muscle groups that will support the prosthesis.
During this period, doctors may also introduce mirror therapy or EMG biofeedback to train muscle signals for myoelectric prosthetic use.
Phase Four: Transition to First Fit
When patients achieve good strength, balance, and confidence, physicians greenlight the first prosthetic fitting.
Thanks to pre-hab, this transition happens faster and smoother. The limb tolerates the socket better, the patient adapts more quickly, and walking or gripping feels less foreign.
Doctors then adjust rehabilitation goals to integrate prosthetic training seamlessly into ongoing therapy.
How Pre-Hab Reduces Time to First Fit
Maintaining Limb Shape and Volume
Swelling and volume changes are common after surgery. Without early management, these fluctuations delay socket fabrication.
Pre-hab techniques like compression wrapping, gentle massage, and controlled activity help stabilize limb volume sooner.
When the limb reaches a consistent shape faster, the prosthetist can take accurate measurements earlier, reducing waiting time for the first fit.
Reducing Complications and Delays
Patients who remain inactive for long periods are prone to joint stiffness, infection, and muscle contractures.
Pre-hab keeps tissues healthy and circulation strong, reducing these risks.
Fewer complications mean fewer hospital visits—and faster progression to prosthetic evaluation.
Enhancing Surgical Outcomes
Physicians who integrate pre-hab principles even before amputation (known as pre-surgical pre-hab) often see smoother recoveries.
By strengthening muscles and improving cardiovascular health before surgery, patients heal better and tolerate post-surgical therapy with fewer setbacks.
This proactive approach transforms recovery into a predictable, streamlined process.
Boosting Patient Confidence
Fear and anxiety can slow progress as much as physical limitations. Pre-hab gives patients something tangible to focus on—movement, progress, and participation.
When they realize they can move safely, confidence replaces fear. This psychological shift accelerates their willingness to engage in therapy post-fit, cutting down adjustment time.
The Multidisciplinary Power of Pre-Hab
Why Pre-Hab Needs a Team
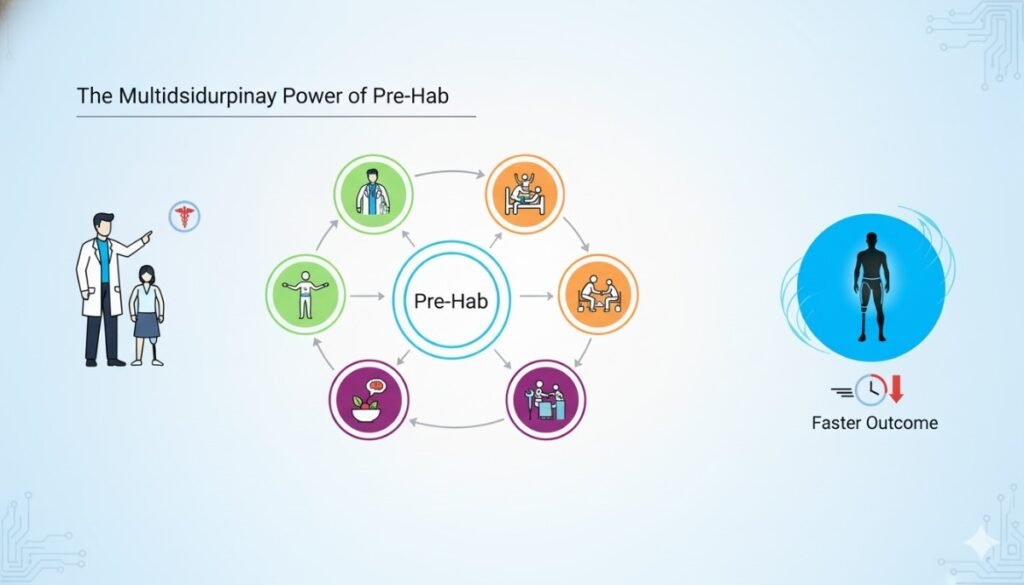
Pre-habilitation is never a one-person job. It’s a collaboration that thrives when surgeons, physiatrists, prosthetists, physical therapists, and psychologists work in sync.
Each member of this team plays a unique role. Surgeons ensure surgical recovery is complete. Physiatrists design the functional roadmap. Therapists lead physical and emotional conditioning. Prosthetists plan for the eventual fitting.
When communication flows smoothly among them, the patient’s journey becomes faster, safer, and more rewarding.
The Surgeon’s Responsibility
The surgeon initiates the process by providing medical clearance for pre-hab activities. They monitor healing, prevent complications, and ensure the residual limb is ready for controlled motion.
In ideal setups, surgeons refer patients to pre-hab specialists even before discharge. This early handover ensures no time is lost between surgery and rehabilitation.
By maintaining regular contact with the rehab team, surgeons help track healing progress and adapt protocols in real time.
The Physiatrist’s Guidance
Physiatrists act as the bridge between medicine and movement. They evaluate muscle tone, joint function, and overall stamina before designing a personalized pre-hab plan.
Their expertise ensures exercises are medically safe yet challenging enough to stimulate progress. They also help monitor cardiovascular fitness, ensuring patients can tolerate increasing levels of activity.
In many centers, physiatrists serve as the primary coordinators, ensuring that every professional involved follows a unified strategy.
The Prosthetist’s Perspective
Even though fitting happens later, prosthetists contribute early by advising on limb shaping, skin care, and desensitization routines.
Their guidance on maintaining proper limb volume and alignment helps prevent socket-fitting challenges later.
They may also introduce patients to educational models or digital simulations, explaining how prosthetic systems work. This knowledge turns anticipation into preparation rather than anxiety.
The Therapist’s Role
Physical and occupational therapists are the heart of pre-hab. They train patients in controlled movement, balance, and daily activity modifications.
They teach exercises that preserve strength and flexibility, using resistance bands, therapy balls, or mirror feedback to maintain engagement.
Occupational therapists help patients adapt psychologically, encouraging independence in grooming, dressing, and self-care even before prosthetic fitting.
The Psychologist’s Support
Amputation can trigger depression, anxiety, and identity loss. Psychologists in pre-hab programs provide emotional grounding during this vulnerable phase.
They help patients process grief, rebuild confidence, and set realistic recovery goals.
By managing fear and frustration early, psychologists ensure that mental resilience grows alongside physical readiness.
Building Trust Through Communication
The Power of Clear Dialogue
For many patients, amputation is uncharted territory. They depend on physicians not only for medical care but also for reassurance and understanding.
When doctors communicate clearly about pre-hab—what it is, why it matters, and what to expect—it transforms fear into participation.
Explaining every step helps patients see progress as part of a bigger journey rather than isolated exercises.
Setting Realistic Expectations
Pre-hab doesn’t promise instant miracles. Doctors must emphasize that progress takes time and that small daily efforts matter most.
When expectations are grounded, motivation stays steady. Overpromising results can lead to disappointment; being transparent builds trust and commitment.
Physicians who use visuals, diagrams, or videos often find patients more engaged and confident about the process.
Creating Emotional Safety
Recovery is as much emotional as it is physical. Some patients may feel embarrassed by their limitations or frustrated by slow progress.
A physician’s empathy can make all the difference. Listening, validating feelings, and celebrating even the smallest achievements builds emotional safety.
When patients feel understood, they stay consistent—and consistency drives success.
Empowering the Family
Family members play a key role in supporting pre-hab at home. Doctors who involve them early help create a positive environment for recovery.
Teaching families how to assist without overprotecting helps patients maintain independence. It turns pre-hab from a clinical exercise into a shared family victory.
Families who see the patient’s effort and improvement often become their strongest motivators.
Real-Life Insights: How Pre-Hab Changes Everything
The Case of the Young Athlete
A 24-year-old football player lost his lower leg in a road accident. Instead of waiting for full wound healing, his doctor initiated light pre-hab within two weeks.
The focus was on breathing exercises, upper-body strength, and hip control.
Within three months, his limb was ready for fitting with minimal volume fluctuation. Because his muscles remained strong, he adapted to his prosthesis quickly, walking independently within six months.
His progress wasn’t luck—it was preparation.
The Homemaker Who Found Her Rhythm Again
A 48-year-old homemaker underwent a below-elbow amputation due to severe infection. Her surgeon referred her to a pre-hab team immediately after surgery.
She began with gentle shoulder mobility and light resistance training. Emotional counseling helped her manage fear and sadness.
By the time her myoelectric hand was fitted, her muscle signals were clear and strong.
Her doctor later remarked that the time from surgery to independent use was nearly half that of similar cases without pre-hab.
The Senior with Renewed Confidence
A 65-year-old man lost his leg due to diabetes. Initially, he was hesitant to move, fearing pain and instability.
His physician introduced a slow, supervised pre-hab routine focusing on balance and joint flexibility. As his confidence grew, he began participating actively in daily sessions.
When his prosthesis was ready, he took his first steps with surprising ease.
Pre-hab didn’t just prepare his body—it restored his belief in his ability to recover.
The Indian Context: Making Pre-Hab Accessible
Challenges in the Current System

In India, pre-hab remains underutilized. Many hospitals still follow a post-rehabilitation model, starting therapy only after healing is complete.
This delay extends the recovery timeline and increases dependency. Limited awareness among healthcare professionals and patients often contributes to the gap.
But that’s beginning to change. As evidence grows, physicians across India are recognizing pre-hab as a critical phase rather than an optional add-on.
The Role of Local Manufacturing and Innovation
Indian prosthetic manufacturers like RoboBionics are making early rehabilitation programs more practical and affordable.
Because devices like the Grippy™ Bionic Hand and other locally made prosthetics cost a fraction of imported ones, hospitals can now integrate training earlier without budget constraints.
Affordability allows doctors to introduce real prosthetic interaction during pre-hab—patients can practice muscle control or simulated grips, even before full fitting.
This early exposure helps shorten the mental and physical learning curve.
Training Programs for Physicians and Therapists
RoboBionics regularly collaborates with medical colleges and rehabilitation centers to conduct workshops on pre-hab and early prosthetic readiness.
These sessions train doctors on how to identify candidates, design protocols, and use EMG biofeedback tools effectively.
By equipping medical professionals with practical skills, these programs strengthen India’s overall rehabilitation infrastructure.
Rural Outreach and Accessibility
For patients in remote areas, consistent therapy can be challenging. That’s why RoboBionics supports tele-rehabilitation and mobile prosthetic units.
Through video-guided exercises and virtual check-ins, physicians can oversee pre-hab progress from afar.
This digital bridge ensures that even rural patients can begin pre-hab early, cutting down travel time and waiting periods for prosthetic readiness.
Data-Driven Validation
One of the strongest advantages of integrating pre-hab is measurability.
Doctors can track improvements using functional tests like AMPnoPRO or TUG scores, comparing pre- and post-fit performance.
In hospitals using RoboBionics’ clinical tracking systems, patients who completed pre-hab programs showed faster socket tolerance and better walking endurance.
Numbers confirm what intuition already tells us—preparation pays off.
How RoboBionics Integrates Pre-Hab Philosophy
Beyond Technology—A Human Mission
At RoboBionics, our vision goes far beyond building prosthetic limbs. We aim to build confidence, purpose, and freedom.
Pre-habilitation aligns perfectly with this mission. It transforms prosthetic care from a reactive process into a proactive journey of empowerment.
Our devices are designed to complement this philosophy—lightweight, responsive, and intuitive enough for early introduction.
The Grippy™ Advantage
Our flagship Grippy™ Bionic Hand is engineered to respond seamlessly to natural muscle signals. This makes it ideal for early-stage training and biofeedback exercises.
With Sense of Touch™ technology, patients can experience controlled grip feedback during pre-hab sessions. This accelerates muscle coordination and emotional connection to the prosthesis.
When the time for fitting arrives, the patient is already familiar with the feel of movement—making the first use smooth and instinctive.
Collaborating with Doctors and Hospitals
We partner closely with surgeons, physiatrists, and therapists to integrate pre-hab into their patient care systems.
Our approach is collaborative: providing training materials, technical support, and feedback mechanisms that help physicians monitor patient progress easily.
This partnership ensures every patient benefits from structured preparation, regardless of where they begin their journey.
Making Pre-Hab Affordable
Affordability remains at the core of our mission. By manufacturing 60 out of 64 components in India, we’ve reduced dependency on imported technology.
This localization not only lowers costs but also ensures faster availability of replacement parts and customization.
It’s why more hospitals can now recommend early prosthetic readiness confidently—without financial hesitation.
Physician-Guided Pre-Hab Exercises
Building Strength from the Core
The foundation of every successful prosthetic journey lies in core stability. Physicians often begin pre-hab by focusing on the muscles that keep the trunk steady and aligned.
For lower-limb amputees, these include the abdominals, back extensors, and gluteal muscles. For upper-limb cases, posture and shoulder stability become the focus.
Simple exercises like seated torso rotations, pelvic tilts, or bridging help keep the spine and hips strong. A stable core ensures that when patients start walking or lifting with a prosthesis, their body can support the new motion naturally.
Preparing the Residual Limb
Before a prosthesis can be worn comfortably, the residual limb must be strong, supple, and well-shaped.
Doctors and therapists work together to design exercises that encourage blood flow and maintain skin elasticity. Patients are taught gentle stretching and massaging techniques to keep tissues mobile.
Desensitization routines, such as tapping or rubbing with different textures, help the limb adjust to future socket pressure. Compression wrapping is introduced gradually to manage swelling and promote shaping.
The result is a limb that’s not just healed, but conditioned for the next phase.
Enhancing Upper-Body Strength
For lower-limb amputees, upper-body strength becomes the key to balance and movement. Physicians prescribe progressive resistance exercises using bands or light weights.
Shoulder presses, arm curls, and chair dips help patients regain confidence and power in their arms, which will later aid with transfers, crutch use, or prosthetic control.
These early workouts not only build muscle but also reintroduce a sense of physical capability that many patients feel they’ve lost after surgery.
Balance and Coordination Training
After amputation, the body’s sense of balance shifts dramatically.
Doctors introduce simple yet effective exercises that retrain equilibrium — like seated balance shifts, single-leg stands for below-knee amputees, and supported weight transfers for above-knee cases.
These exercises reeducate the brain to trust movement again. Over time, balance training turns hesitation into confidence, laying the foundation for smooth prosthetic gait later.
Flexibility and Range of Motion
Maintaining flexibility prevents long-term stiffness and contractures. Physicians encourage gentle stretching of the hip flexors, hamstrings, and shoulder joints to keep movement free.
For upper-limb amputees, passive and active-assisted range of motion exercises are vital. These movements prevent the shoulder from tightening, ensuring it stays ready for prosthetic alignment.
Consistent flexibility work also reduces pain and makes socket fitting more comfortable.
Cardiovascular Conditioning
Amputation can significantly reduce physical activity, which in turn affects stamina. Doctors incorporate light cardiovascular conditioning into pre-hab programs.
For example, seated cycling, arm ergometer exercises, or simple breathing drills help maintain endurance without stressing healing tissues.
This aerobic focus not only improves heart health but also boosts oxygen delivery to healing muscles, supporting faster recovery.
EMG Training for Myoelectric Control
For upper-limb amputees, pre-hab often includes EMG (electromyography) training — a process where patients learn to control muscle signals that will later activate their prosthesis.
Small electrodes record muscle contractions on a screen, turning invisible effort into visible feedback.
This helps patients isolate specific muscles and learn intentional control. When the prosthesis arrives, they already know how to communicate with it effectively.
Mental Focus and Visualization
Physicians often guide patients through mental rehearsal — imagining themselves moving, walking, or grasping with their prosthesis.
This mental exercise strengthens neural pathways and primes the brain for coordination. Combined with light meditation and breathing control, it also calms anxiety and enhances emotional resilience during recovery.
In many programs, this balance between mental and physical work defines the patient’s pace of progress.
Tailoring Pre-Hab for Different Cases
Lower-Limb Amputees

For lower-limb cases, pre-hab emphasizes endurance, core balance, and residual limb conditioning.
Doctors focus on preventing contractures by maintaining hip and knee mobility. Early standing tolerance exercises help re-establish confidence in bearing weight, even if partially supported.
Gait simulation training — using parallel bars or virtual reality systems — helps patients understand posture and step rhythm before their first fit.
When fitting begins, the transition from therapy to walking feels fluid and instinctive.
Upper-Limb Amputees
For upper-limb cases, pre-hab centers around control and coordination.
Strengthening the shoulder girdle and maintaining range of motion are top priorities.
Doctors often combine traditional physical therapy with EMG feedback and fine-motor skill exercises, such as manipulating small objects or squeezing stress balls, to preserve dexterity.
Patients are also encouraged to perform bilateral tasks using their sound limb and the residual limb together. This helps balance muscle use and reduces strain later.
Bilateral Cases
Bilateral amputees require special attention because pre-hab must address not just movement but adaptation.
Doctors guide these patients through activities of daily living using assistive tools, helping them gain independence in grooming, feeding, and mobility.
Balance, posture, and emotional confidence become intertwined goals.
By introducing adaptive techniques early, physicians empower patients to reclaim functionality and dignity even before prosthetic fitting.
Pediatric Cases
Children benefit immensely from pre-hab, as their bodies and brains adapt faster than adults.
Physicians keep sessions playful and interactive — using games, balance boards, and storytelling to encourage participation.
For growing children, pre-hab also helps prevent muscle imbalances and ensures natural development of coordination as they transition to prosthetic use.
Early exposure builds acceptance, making prosthetic integration effortless later on.
Geriatric Cases
For older adults, pre-hab must balance caution with confidence.
Physicians focus on safe, low-impact exercises that maintain strength and joint mobility without overexertion.
Balance training and fall prevention become crucial components. Light activity, paired with emotional encouragement, keeps seniors active and engaged, reducing the fear of dependency.
Even small improvements in endurance at this stage lead to major gains during prosthetic training.
Measuring Pre-Hab’s Impact
Objective Outcomes
Doctors track pre-hab progress through measurable outcomes such as the Timed Up and Go (TUG) test, the Six-Minute Walk Test (6MWT), and the Amputee Mobility Predictor (AMPnoPRO).
These benchmarks quantify strength, balance, and readiness for prosthetic fitting.
Patients who undergo structured pre-hab consistently show higher scores and shorter rehabilitation durations. Their first steps or grips often happen weeks earlier than average.
Functional Readiness
Pre-hab patients reach functional readiness faster. Their limbs tolerate socket pressure better, wounds heal more efficiently, and pain levels remain lower.
Doctors note that these patients often require fewer prosthetic adjustments after fitting because their muscles and tissues adapt more smoothly.
This efficiency translates into better long-term outcomes and greater patient satisfaction.
Emotional and Social Impact
Beyond physical metrics, the emotional impact is profound.
Patients who start pre-hab early often report reduced anxiety, higher confidence, and stronger motivation. They approach prosthetic training with optimism instead of fear.
Families, too, feel empowered when they witness progress. The sense of shared achievement strengthens emotional bonds and fosters ongoing support.
Cost and Time Efficiency
By reducing complications and therapy time, pre-hab also lowers overall treatment costs.
Faster recovery means fewer hospital visits, shorter inpatient stays, and quicker return to work or school.
For healthcare systems in India, integrating pre-hab can make prosthetic rehabilitation not only more effective but more sustainable.
Robobionics and the Future of Pre-Hab in India
Redefining the Recovery Path
At Robobionics, we believe recovery begins long before fitting day. Our mission is to equip both physicians and patients with the tools and knowledge needed for proactive rehabilitation.
Through our workshops and partnerships with hospitals, we’re helping pre-hab become a standard part of prosthetic care across India.
Early movement, guided strength, and emotional empowerment form the backbone of our philosophy.
Designed for Early Adaptation
Our prosthetic technologies, including the Grippy™ Bionic Hand and other innovative systems, are built to integrate seamlessly into pre-hab programs.
Their lightweight design and intuitive control systems allow physicians to introduce muscle coordination exercises safely, even during early rehabilitation phases.
Because our devices respond to real human intention, patients can begin practice sooner — learning confidence before dependence.
Collaboration with Physicians
RoboBionics works closely with surgeons, physiatrists, and therapists to create evidence-based pre-hab modules tailored for Indian patients.
We provide training materials, measurement tools, and on-ground support that help doctors implement structured, data-driven programs.
Our shared goal is simple — reduce time to first fit, enhance recovery quality, and make every patient’s first step or first grip a moment of triumph.
Accessibility for All
By manufacturing the majority of our components in India, we make high-quality prosthetics affordable for every region and income group.
This accessibility ensures that pre-hab isn’t just a privilege—it becomes a possibility for anyone in need.
We envision a future where every hospital, large or small, can offer physician-led pre-hab as a core service.
Measuring What Matters
We are continuously gathering clinical data from partner hospitals to study how pre-hab affects recovery time and long-term performance.
Preliminary results show that patients who completed structured pre-hab programs were ready for prosthetic fitting 30–40% faster than those without early preparation.
These numbers confirm what we’ve always believed — that preparation saves time, cost, and emotional strain.
Conclusion: Preparation Is Power
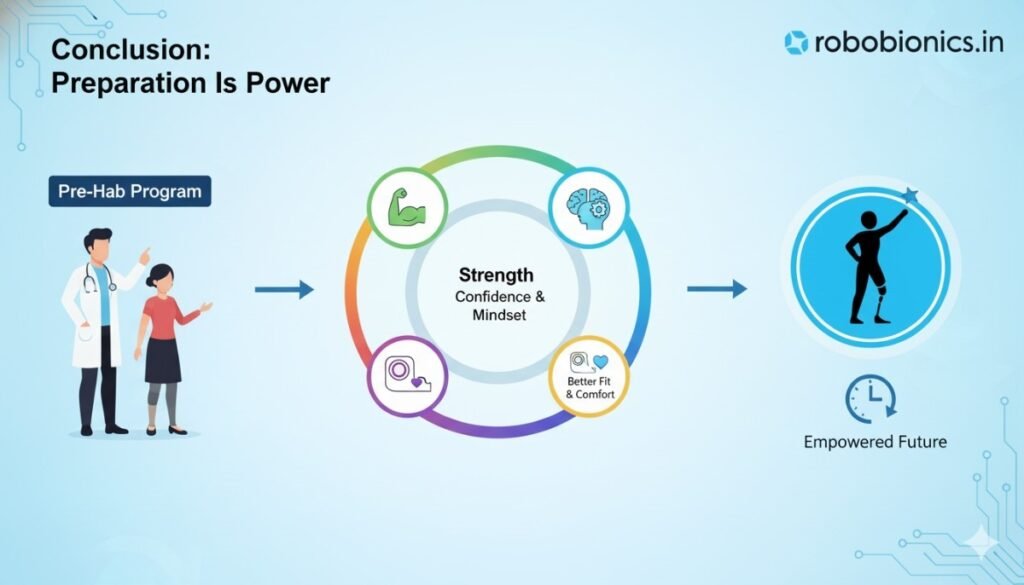
The first fit is more than a medical milestone. It’s a turning point in a person’s story — the moment they move from limitation toward possibility.
Physician-led pre-hab ensures that moment comes sooner, stronger, and smoother. It keeps the body ready, the mind engaged, and the heart determined.
At Robobionics, we stand by one truth: early preparation transforms outcomes. By combining medical expertise with compassionate innovation, we’re helping physicians redefine what recovery looks like.
If you’re a surgeon, physiatrist, or rehabilitation specialist ready to bring early mobility to your patients, we invite you to partner with us.
Book a demo or schedule a consultation at patients.robobionics.in/bookdemo.
Let’s make preparation the first step in every journey — because when doctors lead with readiness, patients walk sooner, stronger, and with dignity.